Contributors

Lily Henderson
Dietitian, My Food Bag
Subscribe to our newsletter
Thank you! Your submission has been received!
Oops! Something went wrong while submitting the form.


Diabetes doesn’t affect men and women in the same way. Hormones naturally fluctuate throughout the menstrual cycle, during menopause, and in response to stress – all of which can impact how your body handles blood sugar.
By understanding your hormones and how they influence your blood sugar levels, you can make more better food choices – helping to reduce your risk of type 2 diabetes.
NZ Registered Dietitian Lily Henderson arms you with simple science-backed nutrition shifts to set you up for success.
Insulin is a hormone that helps to move sugar (or glucose) from your blood into your cells – but it doesn't work alone. Female hormones influence how your body manages your blood sugar levels:
While diabetes affects both men and women, women face unique sex-specific risk factors due to hormonal differences.
These include:
Gestational diabetes: which is when blood sugar levels are raised during pregnancy. Women with gestational diabetes have an 8-10 times higher risk of developing type 2 diabetes (1).
Polycystic ovary syndrome (PCOS): affects how the body uses and responds to insulin, making it harder to keep blood sugar levels stable. Women with PCOS are three times more likely to develop type 2 diabetes than women without the condition (2).
Perimenopause & menopause: as oestrogen levels decline, the body becomes less responsive to insulin, making it harder to manage blood sugar and increasing fat storage around the tummy area. This shift increases the risk of type 2 diabetes and diabetes-related heart disease (3).
Heart disease risk: without diabetes, women tend to have a lower risk of heart disease than men – largely due to the protective effects of oestrogen. But with diabetes, that advantage disappears. In fact, diabetes raises the risk of heart disease more in women than in men (4,5).
Social pressures: body image pressures, disordered eating, or under-fuelling (especially in younger or active women) can increase stress hormones like cortisol and lead to fluctuating blood sugar levels.
No matter your age or stage you don’t need an extreme diet, detox or fancy hormone balancing supplement. It’s also normal for your blood sugar levels to rise and fall throughout the day.
Here are my simple, science-backed habits:
Tick off each nutrient when you build your plate
At each meal, aim to include:
A source of protein (e.g. eggs, fish, meat, chicken, tofu, yoghurt, cottage cheese)
A source of dietary fibre (e.g. legumes, vegetables, fruit, whole grains)
A healthy fat (e.g. avocado, olive oil, nut butter, nuts, seeds)
These nutrients work together to slow digestion, support stable blood sugars and keep energy levels steady.
Swap refined carbs to quality carbs
Carbs are not the enemy – they fuel your brain, muscles, and menstrual cycle.
The trick is to choose a range of better-quality carbs and ensure they don’t dominate your plate.
Focus on quality, high-fibre carbs like:
Eat regularly – but not constantly
Constant grazing makes it harder to manage your blood sugar levels.
We all have days where we’re extra hungry or in the mood to snack but it’s important to find a rhythm that works for you. Set yourself up for the day with a nourishing breakfast and plan to eat every 3-5 hours with filling, balanced meals.
Signs that your day of eating may be impacting your blood sugar levels:
Give yourself permission to eat enough
Not skipping meals can help to manage your blood sugar levels and prevent hunger. It also reduces the likelihood of overeating later.
Give yourself permission to eat consistent, nourishing meals to help your body feel safe and stable.
Build in lifestyle habits that support optimal hormonal health
This could include getting morning light each day to support your circadian rhythm, gentle daily movement to support your nervous system or prioritising your sleep each night to lower stress hormones and to support blood sugar management.
Rather than making several big changes, just one or two simple ones will be easier to stick to and more likely to become a habit over time.
What does a balanced plate look like?
Try these super simple and delicious meal combinations:
.jpg)
Try these blood-sugar friendly snack pairings:
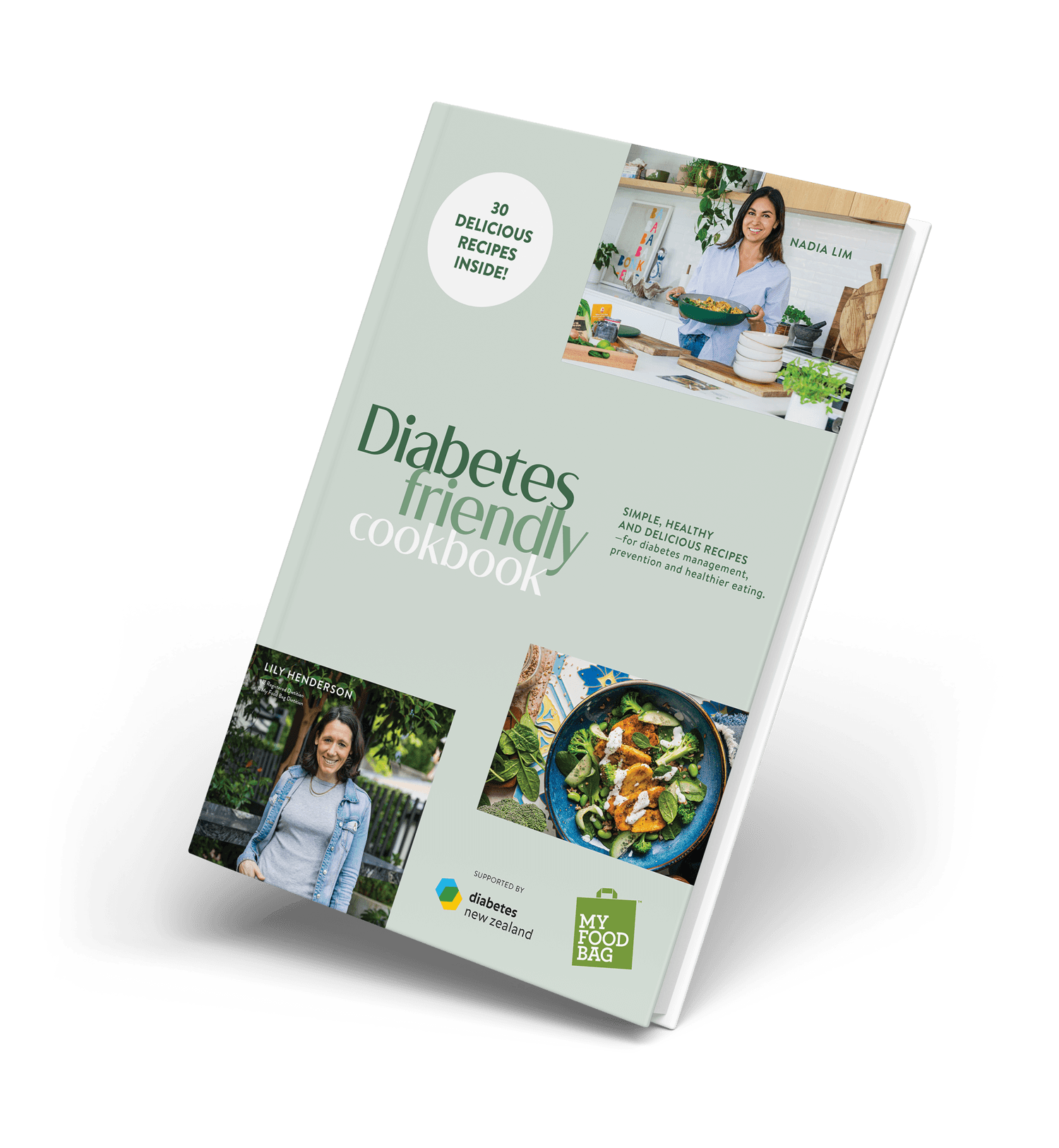
Download a free My Food Bag Diabetes Friendly e-book. Whether you’re managing type 2 diabetes, working to manage your blood sugar levels, or simply looking to eat better, inside you’ll find a collection of 30 simple, nourishing and delicious recipes that anyone can enjoy.
References